Gluck et al in 1971 discovered that fetal lung maturity was found to be related to the surface active phospholipid lecithin. When compared with another phospholipid, sphingomyelin, the lecithin/ sphingomyelin ratio was found to be predictive of severe idiopathic respiratory distress syndrome.
Ultrasound guidance was started to be employed in amniocentesis with reports from Jens Bang and Allen Northeved from Copenhagen in 1972, where they worked with Hans Hendrik Holm at the Gentofe Hospital, a center which became famous of interventional imaging.
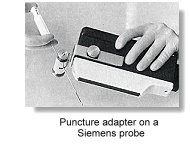
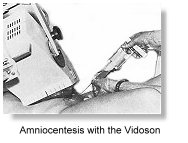 As early as 1967, and basing on the Vidoson, Hofmann and Hollander in Germany had discussed the importance of placental localization using ultrasound before amniocentesis. Jens Bang and Allen Northeved in Copenhagen described ultrasound-guided amniocentesis in 1972. In the mid 1970s to early 80s, genetic amniocentesis was largely performed under static B-scan ultrasound guidance. An ultrasound scan was performed to locate a feasible pocket of amniotic fluid before a tap, which was done basically without actually seeing the needle tip going into the fluid pocket. With the advent of real-time scanners, a small number of centers had in the late 1970s started to perform amniocentesis by simultaneously visualizing the puncture needle tip on the scanner monitor. One such pioneer was the Birnholz group at Harvard who used an early phased array for the purpose. Needle-guide adapters soon became available from ultrasound manufacturers which could be coupled to the linear array or phased array sector probes where the needle passed through a fixed path either parallel or at an angle to the ultrasonic beam. These were cumbersome to use however, particularly in a busy setting. They also had serious problem of keeping the equipment sterile. The adapters may also increase the risk of traumatisation as it did not allow for the 'desired' and sensitive placement of needles.
As early as 1967, and basing on the Vidoson, Hofmann and Hollander in Germany had discussed the importance of placental localization using ultrasound before amniocentesis. Jens Bang and Allen Northeved in Copenhagen described ultrasound-guided amniocentesis in 1972. In the mid 1970s to early 80s, genetic amniocentesis was largely performed under static B-scan ultrasound guidance. An ultrasound scan was performed to locate a feasible pocket of amniotic fluid before a tap, which was done basically without actually seeing the needle tip going into the fluid pocket. With the advent of real-time scanners, a small number of centers had in the late 1970s started to perform amniocentesis by simultaneously visualizing the puncture needle tip on the scanner monitor. One such pioneer was the Birnholz group at Harvard who used an early phased array for the purpose. Needle-guide adapters soon became available from ultrasound manufacturers which could be coupled to the linear array or phased array sector probes where the needle passed through a fixed path either parallel or at an angle to the ultrasonic beam. These were cumbersome to use however, particularly in a busy setting. They also had serious problem of keeping the equipment sterile. The adapters may also increase the risk of traumatisation as it did not allow for the 'desired' and sensitive placement of needles.

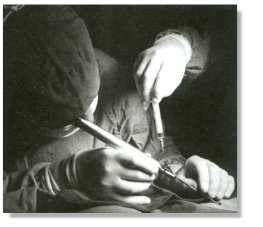
 Many centers started to do it freehand with an assistent holding onto the transducer probe that was commonly wrapped in a sterile adhesive drape. In 1984, Holzgreve in Basel, Switzerland described a large series of over 3000 'freehand' amniocentesis with low complication rate. Similar experience was also reported by Platt in Los Angeles, who emphasised on the need for the transducer probe to be manipulated by the same operator which resulted in better hand-eye co-ordination. In the following year, Romero at Yale formally described the single operator two-hands technique in amniocentesis and the reduction in the number of multiple taps and bloody taps associated with the procedure. Most centers soon adopted the single operator technique, which had become popular because of its convenience and effectiveness. Newer needles were marketed with special external coating and echo-luminence to enhance needle placement.
Many centers started to do it freehand with an assistent holding onto the transducer probe that was commonly wrapped in a sterile adhesive drape. In 1984, Holzgreve in Basel, Switzerland described a large series of over 3000 'freehand' amniocentesis with low complication rate. Similar experience was also reported by Platt in Los Angeles, who emphasised on the need for the transducer probe to be manipulated by the same operator which resulted in better hand-eye co-ordination. In the following year, Romero at Yale formally described the single operator two-hands technique in amniocentesis and the reduction in the number of multiple taps and bloody taps associated with the procedure. Most centers soon adopted the single operator technique, which had become popular because of its convenience and effectiveness. Newer needles were marketed with special external coating and echo-luminence to enhance needle placement.
The Benacerraf group reported early amniocentesis (11-14 weeks) in 1988, following some initial reports from Hanson et al. in 1987. In 1990, the Benacerraf group reported an early fetal loss rate of over 2.3%. Several important reviews in the mid-90s confirmed this high incidence of fetal loss. For this reason, the practice was not met with general acceptance.
Fetoscopy and fetal blood sampling
The first attempts at fetoscopy were carried out by Westin in 1954 using a 10 mm diameter hysteroscope introduced through the cervix of patients who were to have therapeutic abortions between 14 and 18 weeks. A transabdominal approach was used by Mandelbaum et al in 1967 during attempts at intrauterine fetal transfusion for haemolytic disease. Fetal skin samples were obtained prior to termination of pregnancy by Valenti in 1972, using a 5mm needlescope which he modified from an 18 French pediatric cystoscope and which he called an endoamnioscope. The term Fetoscopy was introduced by Scrimgeour in 1973. He exposed the uterus at laparotomy and introduced a 2.2 mm needlescope to view the amniotic cavity and fetus. The procedure was performed in six women whose offspring were at high risk of recurring fetal neural tube defect. Three healthy infants were delivered but a fourth had spina bifida.
 Valenti in 1973 used the 'endoamnioscope' and reported the first aspiration of fetal blood and the diagnosis of haemoglobinopathy. The newer Dyonics® Needlescope became available in the following year, which was 1.7mm in diameter with a 2mm cannula. General anaesthetics was not required for its use.
Valenti in 1973 used the 'endoamnioscope' and reported the first aspiration of fetal blood and the diagnosis of haemoglobinopathy. The newer Dyonics® Needlescope became available in the following year, which was 1.7mm in diameter with a 2mm cannula. General anaesthetics was not required for its use.
 Pioneering work came from Hobbins and Mahoney at Yale and Patrick, Perry and KInch in Canada in the same year. Initial work was performed on patients between 15 and 20 weeks of gestation. The use of sonography prior to the procedure was much emphasised. Fetal blood aspiration was performed via a 27-gauge needle inserted through a special cannula allowing aspiration under direct vision. The special cannula was named the Hobbins cannula. It was noted that there was no evidence of any vessel trauma at postmortem examination and blood samples were more successfully obtained after 18 weeks and peripheral parts better visualized than central ones.
Pioneering work came from Hobbins and Mahoney at Yale and Patrick, Perry and KInch in Canada in the same year. Initial work was performed on patients between 15 and 20 weeks of gestation. The use of sonography prior to the procedure was much emphasised. Fetal blood aspiration was performed via a 27-gauge needle inserted through a special cannula allowing aspiration under direct vision. The special cannula was named the Hobbins cannula. It was noted that there was no evidence of any vessel trauma at postmortem examination and blood samples were more successfully obtained after 18 weeks and peripheral parts better visualized than central ones.
 In 1977, Hobbins and Mahoney reported successful exclusion of beta-thalassemia and diagnosis of sickle cell disease without aparent risk to the mother and fetus. Other important workers included Alter and Nathan, and Fairweather in London. Rodeck and Campbell reported the diagnosis of spina bifida using this method. In 1979 the group reported a success rate of obtaining pure blood samples of 94% in 51 attempts. They introduced the method of aspirating from one of the larger vessels at the base of the cord. Most investigators started with the diagnosis of haemoglobinopahies, in which maternal cell contamination did not affect the accuracy of the results
In 1977, Hobbins and Mahoney reported successful exclusion of beta-thalassemia and diagnosis of sickle cell disease without aparent risk to the mother and fetus. Other important workers included Alter and Nathan, and Fairweather in London. Rodeck and Campbell reported the diagnosis of spina bifida using this method. In 1979 the group reported a success rate of obtaining pure blood samples of 94% in 51 attempts. They introduced the method of aspirating from one of the larger vessels at the base of the cord. Most investigators started with the diagnosis of haemoglobinopahies, in which maternal cell contamination did not affect the accuracy of the results
 Other reported diseases diagnosed via fetoscopy included haemophilia (1979, Firsheim), chronic granulomatous disease (1979, Newburger), galactosaemia (1979, Fensom), and Tay-Sachs disease (1979, Perry). Fetal skin biopsy successfully diagnosed congenital bullous ichthyosiform erythroderma ichthyosis by the Golbus group in San Francisco in 1979 and epydermolysis bullosa letalis by the Rodeck group in 1980. In 1982, the Rodeck group reported fetal liver biopsy for prenatal diagnosis of ornithine carbamyltransferace deficiency.
Other reported diseases diagnosed via fetoscopy included haemophilia (1979, Firsheim), chronic granulomatous disease (1979, Newburger), galactosaemia (1979, Fensom), and Tay-Sachs disease (1979, Perry). Fetal skin biopsy successfully diagnosed congenital bullous ichthyosiform erythroderma ichthyosis by the Golbus group in San Francisco in 1979 and epydermolysis bullosa letalis by the Rodeck group in 1980. In 1982, the Rodeck group reported fetal liver biopsy for prenatal diagnosis of ornithine carbamyltransferace deficiency.
 Fetoscopic guided Laser occlusion of chorioangiopagous vessels (FLOC) was first pioneered by De Lia in 1988 at the University of Utah for the treatment of the Twin-to-Twin-Transfusion Syndrome (TTTS) . Nicolaides at King's and Ville in France introduced the technique to Britain and Europe in 1991. It is now standard treatment for this condition in many perinatal centers.
Fetoscopic guided Laser occlusion of chorioangiopagous vessels (FLOC) was first pioneered by De Lia in 1988 at the University of Utah for the treatment of the Twin-to-Twin-Transfusion Syndrome (TTTS) . Nicolaides at King's and Ville in France introduced the technique to Britain and Europe in 1991. It is now standard treatment for this condition in many perinatal centers.
After fetoscopy, ultrasound-guided pure fetal blood cordocentesis was pioneered in
France in 1983 by Daffos. Pure fetal blood was aspirated in-utero at around 18 weeks from the umbilical vein near the placental insertion of the cord using a twenty gauge needle under ultrasound guidance. Their group reported the first case of Haemophilia A diagnosed in-utero by this method. The procedure was also popularised around the same time in England by the Campbell
and Rodeck group at King's College Hospital. The Hobbins group at Yale described their technique in 1985 and called the procedure percutaneous umbilical blood sampling (PUBS). This replaced blood sampling via fetoscopy which the group had pioneered in 1974.
 Nicolaides at King's developed the single operator two-hands method and became a leading figure in cordocentesis exploring many important aspects of fetal
physiology and pathophysiology. With the advent of color flow mapping, the technique has become even more accessible. In 1988, Nicolini, working with Rodeck at the Queen Charlotte's Maternity Hospital in London, first described fetal blood sampling from the intrahepatic portion of the umbilical vein in the fetus, as an alternative procedure in cases where cord needling was unsuccessful.
Nicolaides at King's developed the single operator two-hands method and became a leading figure in cordocentesis exploring many important aspects of fetal
physiology and pathophysiology. With the advent of color flow mapping, the technique has become even more accessible. In 1988, Nicolini, working with Rodeck at the Queen Charlotte's Maternity Hospital in London, first described fetal blood sampling from the intrahepatic portion of the umbilical vein in the fetus, as an alternative procedure in cases where cord needling was unsuccessful.
In the late 1980s fetoscopy has mainly been reserved for tissue or organ sampling, and fetal blood sampling are always done via the ultrasonic-guidance needle procedure. The commonest indication of fetal blood sampling had evolved to become one of quick confirmation of abnormal karyotype in the 22-24 weeks fetus, when a chromosomal abnorrmality has been suggested on ultrasound scan.
In 1990, Cullen, Reece, Whethaam and Hobbins described the new technique of "Embryoscopy', a transabdominal thin gauge embryo-fetoscopy procedure in the first trimester. Quintero, Abuhamad, Hobbins and Mahonney reviewed the clinical application of the procedure in 1993 and reported the early prenatal diagnosis of a case of Meckel Gruber Syndrome using this technique.
Chorionic villus Sampling (Biopsy)
 In 1968 Mohr in Scandinavia introduced the concept of antenatal genetic diagnosis using sampled chorionic villi. He performed transcervical biopsy of the chorion under direct endoscopic vision, using a straight 5mm endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding, infection and failed culture. The approach was slowly abandoned in the midst of increasing safety from mid-trimester amniocentesis. Kullander and Sandahl in 1973 and Hahnemann in 1974 reported fetal chromosome analysis from transcervical placental biopsy prior to termination in early pregnancies. The first successful prenatal diagnostic use of chorionic villi biopsy was apparently reported in 1975 from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China, where fetal sex was diagnosed for the purpose of sex pre-selection. This was reported in the first issue of the (new) Chinese Medical Journal. They performed blind aspirations using a 3mm metal cannula on a group of 100 patients. When a soft resistence was met, a smaller internal tube was advanced further and placental material obtained by syringe suction. They claimed to have 6 wrong diagnosis out of 99 successful attempts and only 4 prenatal losses. Investigators in the United States were, however unable to duplicate the results and the idea of first trimester antenatal diagnosis was again shelfed for some time.
In 1968 Mohr in Scandinavia introduced the concept of antenatal genetic diagnosis using sampled chorionic villi. He performed transcervical biopsy of the chorion under direct endoscopic vision, using a straight 5mm endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding, infection and failed culture. The approach was slowly abandoned in the midst of increasing safety from mid-trimester amniocentesis. Kullander and Sandahl in 1973 and Hahnemann in 1974 reported fetal chromosome analysis from transcervical placental biopsy prior to termination in early pregnancies. The first successful prenatal diagnostic use of chorionic villi biopsy was apparently reported in 1975 from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China, where fetal sex was diagnosed for the purpose of sex pre-selection. This was reported in the first issue of the (new) Chinese Medical Journal. They performed blind aspirations using a 3mm metal cannula on a group of 100 patients. When a soft resistence was met, a smaller internal tube was advanced further and placental material obtained by syringe suction. They claimed to have 6 wrong diagnosis out of 99 successful attempts and only 4 prenatal losses. Investigators in the United States were, however unable to duplicate the results and the idea of first trimester antenatal diagnosis was again shelfed for some time.
Apparently with the advent of ultrasound and advancement in molecular genetics the desire for an earlier antenatal diagnosis was rekindled. Kazy et at. in 1980, in the USSR reported fetal sexing and enzyme assay on chorion biopsies taken at 6 -12 weeks' gestation, using either an endoscopic or ultrasound-guided approach. Biopsy forceps were used instead of cannulas. This was the first report in the literature of using ultrasound guidance during chorion sampling. Niazi et al. in 1981 at the St. Mary's Hospital, London reported improved methods for culturing of fibroblasts from trophoblast villi.
 In 1983, Ward in London performed transcervical chorionic sampling under ultrasonic guidence using a 1.5 mm malleable polyethylene catheter and syringe suction. His group reported 67% sampling success rate, including 7 patients for the diagnosis of haemoglobinopathies. The Brambati group in Milan demonstrated in 1983 that with ultrasonic guidance, success rate of obtaining chorionic material rose from 75% to 96%. Brambati used a 1.5mm polyethylene tube with a soft stainless steel malleable obturator inserted into the 1 mm internal barrel. This design has been the most common design in use today. Other workers like Dumez in Paris used a simple 2 mm biopsy forceps. The Simoni and Brambati group in Milan described in 1983 a technique for direct chromosome and biochemical analysis on first trimester chorionic villi (direct prep), without preliminary culture. Chorionic villi were obtained by aspiration or direct biopsy from the chorion frondosum, at the edge of the placental disc. The inner cytotrophoblastic layer beneath the outer syncytiotrophoblast layer contains actively mitotic cells in freshly sampled villus which could be recovered with their technique. Virtually all analyses could be performed with these fresh whole villus.
In 1983, Ward in London performed transcervical chorionic sampling under ultrasonic guidence using a 1.5 mm malleable polyethylene catheter and syringe suction. His group reported 67% sampling success rate, including 7 patients for the diagnosis of haemoglobinopathies. The Brambati group in Milan demonstrated in 1983 that with ultrasonic guidance, success rate of obtaining chorionic material rose from 75% to 96%. Brambati used a 1.5mm polyethylene tube with a soft stainless steel malleable obturator inserted into the 1 mm internal barrel. This design has been the most common design in use today. Other workers like Dumez in Paris used a simple 2 mm biopsy forceps. The Simoni and Brambati group in Milan described in 1983 a technique for direct chromosome and biochemical analysis on first trimester chorionic villi (direct prep), without preliminary culture. Chorionic villi were obtained by aspiration or direct biopsy from the chorion frondosum, at the edge of the placental disc. The inner cytotrophoblastic layer beneath the outer syncytiotrophoblast layer contains actively mitotic cells in freshly sampled villus which could be recovered with their technique. Virtually all analyses could be performed with these fresh whole villus.
In 1984, Smidt-Jensen and Hahnemann in Copenhagen introduced transabdominal fine-needle villus aspiration under ultrasound guidance. With less chance of infective complications and re-insertions the procedure has become more popular than the transcervical counterpart in many prenatal diagnostic centers. Other adjunctive ultrasonic techniques and modifications were reported by the Brambati and Simoni group in Milan and the Golbus group in San Francisco in 1985. The Golbus group reported in 1986 initial experience with 1000 cases of CVS and reported a fetal loss rate of 3.8% and a 1.7% incidence of chromosome mosaicism not found in the fetus. A much lower miscarriage rate of less than 1.5% was subsequently reported by many other centers making the procedure acceptable for routine use.
References:
Alter, B.P., Modell, C.B., Fairweather, D., Hobbins, J.C., Mahoney, M.J., Frigoletto, F.D., Sherman, A.S. & Nathan, D.G. (1976) Prenatal diagnosis of hemoglobinopathies: a review of 15 cases. New England Journal of Medicine, 295,1437
Benacerraf BR, Greene MF, Saltzman DH, Barss VA, Penso CA, Nadel AS, Heffner LJ, Stryker JM, Sandstrom MM, Frigoletto FD (1988). Early amniocentesis for prenatal cytogenetic evaluation. Radiology 169:3 709-10.
Bevis, D.C.A. (1953). The composition of liquor amnii in haemolytic disease of the newborn. J. Obstet. Gynaecol. Br. Emp., 60,244-51
Cullen MT, Reece EA, Whethaam J, Hobbins JC. (1990) Embryoscopy: Description and utility of a new technique. Am J Obstet Gynecol. 162:82-86.
Daffos, F., Cappella-Pavlovsky, M. and Forestier, F. (1983). Fetal blood sampling via the umbilical cord using a needle guided by ultrasound. Report of 66 cases. Prenat. Diagn., 3,271-7
Daffos F, Kappela Pavlosvky M, Forestier F. (1985) Fetal blood sampling during pregnancy with use of a needle guieded by ultrasound : a study of 606 consecutive cases. Am J Obstet Gynecol 153: 655-60.
Department of Obstetrics and Gynaecology, Tietung Hospital, Anshan, China (1975). Fetal sex prediction by sex chromatin of chorionic villi cells during early pregnancy. Chinese Med. J.,1,117-26
Evans, E.P., Burtenshaw, M.D. and Ford, C.E. (1972). Chromosomes of mouse embryos and newborn young: preparations from membranes and tail tips. Shatin Technol, 47,229-34
Fairweather, D.V.I., Ward, R.H.T. & Modell, B. (1980) Obstetrics aspects of midtrimester fetal blood sampling by needling or fetoscopy. British Journal of Obstetrics and Gynaecology, 87,87
Fuchs, F. and Riis, P. (1956). Antenatal sex determination. Nature (London), 177,330
Gluck, L. and Kulovich, M.V. (1973). Lecithin / sphingomelin ratios in amniotic fluid in normal and abnormal pregnancy. Am. J. Obstet. Gynecol., 115,539-46
Golbus, M.S., Sagebiel, R.W., Filly, R.A., Gindhart, T.D. & Hall, J.G. (1979a) Prenatal diagnosis of congenital bulllous ichthyosiform erythroderma (epidemolytic hyperkeratosis by fetal skin biopsy. New England Journal of Medicine, 302,93
Gobus, M.S., Stephens, J.D., Mahoney, M..J., Hobbins, J.C., Haseltine, F.P., Caskey, C.T. & Banker, B.Q. (1979b) Failure of fetal creatinine phospokinase as a diagnostic indicator of Duchenne muscular dystrophy. New England Journal of Medicine, 300,860
Hahnemann, N. (1974). Early prenatal diagnosis: a study of biopsy techniques and cell culturing from extra-embryonic membrane. Clin. Genet, 6,294-306
Hobbins, J.C. and Mahoney, M.J. (1974). In utero diagnosis of haemoglobinopathies. Technique of obtaining fetal blood. N. Engl. J. Med., 290,1065
Hobbins, J.C. & Mahoney, M.J. (1977) Fetoscopy in continuing pregnancies. American Journal of Obstetrics and Gynecology, 129,440
Kan, Y.W., Dozy, A.M., Alter, B.P., Frigoletto, F.D. and Nathan, G.G. (1972). Detection of the sickle cell gene in the human fetus. Potential for intrauterine diagnosis of sickle cell anaemia. N. Engl. J. Med., 287,1
Kan, Y.W., Vanenti, C., Guidotti, R, Carnazza, V. and Rieder, R.F. (1974). Fetal blood-sampling in utero. Lancet, 1,79
Kazy Z, Stygar AM, Bakharev VA (1980) Chorionic biopsy under immediate realtime (ultrasonic) control. Orv Hetil 121:2765.
Kazy Z, Rozovsky IS, Bakharev VA (1982) Chorionic biopsy in early pregnency. A method of early prenatal diagnosis for inherited disorders. Prenat Diagn. 2:39.
Kullander, S. and Sandahl, B. (1973). Fetal chromosome analysis after transcervical placental biopsies during early pregnancy. Acta Obstet. Gynaecol. Scand., 52,355-9
Liley, A.W. (1961). Liquor amnii analysis in management of pregnancy complicated by rhesus sensitization. Am. J. Obstet. Gynecol., 82,1359-70
Mandelbaum, B., Pontarelli, D. and Brushenko, A. (1967). Amnioscopy for prenatal transfusion. Am. J. Obstet. Gynecol., 98,1140
Menees, T.O., Millar, J.D. and Holly, L.E. (1930). Amniography. Preliminary report. Am. J. Roentgenol., 24,353-66
Mohr J. (1968) Foetal genetic diagnosis: Development of techniques for early sampling of foetal cells. Acta Pathologica Microbiolabic Scandinavia 73:7377
Milunsky A, Littlefield JW. The prenatal diagnosis of inborn errors of metabolism. (1972) Am Rev Med 23:57.
Nadler HL, Inouye T, Hsia DY (1966) Enzymes in trisomy-18 syndrome. Lancet 4 1:7449 1270
Nadler HL. Antenatal detection of hereditary disorders. (1968) Pediatrics 42:6 912-8.
Nadler HL, Wodnicki JM, Swae MA, O_Flynn ME. (1969) Cultivated amniotic-fluid cells and fibroblasts derived from families with cystic fibrosis. Lancet 12 2:7611 84-5
Nadler HL. (1968) Patterns of enzyme development utilizing cultivated human fetal cells derived from amniotic fluid. Biochem Genet 2:119.
Nadler, H.L. & Gerbie, A.B. (1970) Role of amniocentesis in the intra-uterine diagnosis of genetic defects. New England Journal of Medicine, 282,596
Niazi, M., Coleman, D.V. and Loeffler, F.E. (1981). Trophoblast sampling in early pregnancy. Culture of rapidly dividing cells from immature placental villi. Br. J. Obstet. Gynaecol., 88,1081-5
Nicolaides, K.H., Soothill, P.W., Rodeck, C.H. and Campbell, S. (1986). Ultrasound-guided sampling of umbilical cord and placental blood to assess fetal wellbeing. Lancet, 1,1065-7
Patrick, J.E., Perry, T.B. & Kinch, F.A.H. (1974) Fetoscopy and fetal blood sampling:a
percutaneous approach. American Journal of Obstetrics and Gynecology, 119,539
Perry, T.B., Hechtman, P. & Chow, J.C.W. (1979) Diagnosis of Tay Sachs disease on blood obtained at fetoscopy. Lancet, i,972
Penso CA, Sandtrom MM, Garber MF, Ladoulis M, Stryker JM, Benacerraff BR. (1990) Early amniocentesis : Report of 407 cases with neonatal follow up. Obstet Gynecol 76:1032.
Platt, L.D., Manning, F.A. & Lemay, M. (1978) Real time Bscan directed amniocentesis. American Journal of Obstetrics and Gynecology, 130,700
Quintero RA, Abuhamad A, Hobbins JC, Mahonney MJ. (1993) Transabdominal thin gauge embryo fetoscopy : A technique for early prenatal diagnosis and its uses in tha diagnosis of a case of Meckel Gruber Syndrome. Am J Obstet Gynecol 168:1552-1557
Rodeck, C.H. & Campbell, S. (1978) Early prenatal diagnosis of neural tube defects by ultrasound guided fetoscopy. Lancet, ii,1128
Rodeck, C.H. and Campbell, S. (1978). Sampling pure fetal blood by fetoscopy in second trimester of pregnancy. Br. Med. J., 2,728
Rodeck CH, Patrick AD, Pembrey ME y cols. (1982) Fetal liver biopsy for prenatal diagnosis of ornithine carbamyltransferace deficiency. Lancet 1:189-194.
Rodeck CH, Eadi RAJ, Gosden CM. (1980) Prenatal diagnosis of epydermolysis bullosa letalis. Lancet 1:949-952.
Rodeck, C.H. and Campbell, S. (1979). Umbilical cord insertion as source of pure fetal blood for prenatal diagnosis. Lancet, 1,1244
Romero R, Jeanty P, Reece EA, Grannum P, Bracken M, Berkowitz R, Hobbins JC. (1985) Sonographically monitored amniocentesis of decrease intraoperative complications. Obstet Gynecol 65:426.
Scrimgeour, J.B. (1973). Other techniques for antenatal diagnosis. In Emery, A.E.H. (ed.) Antenatal Diagnosis of Genetic Disease, p. 49. (Edinburgh: Churchill Livingstone)
Simoni, G., Brambati, B., Danesino, C., Rossella, F., Terzoli, G.L., Ferrari, M. and Fraccaro, M. (1983). Efficient direct chromosome analysis and enzyme determinations from chorionic villi samples in the first trimester of pregnancy. Hum. Genet., 63,349-57
Smith, A.D., Wald, N.J., Cuckle, M.S., Stirrat, G.M., Bobrow, M. and Lagercantz, H. (1979). Amniotic fluid acetylcholinesterase as a possible diagnostic test for neural tube defects in early pregnancy. Lancet, 1,686-8
Smidt-Jensen S, Hahnemann N, Jensen PKA, et al (1984) Experience with find needle biopsy in the first trimester-an alternative to amniocentesis. Clin Genet 26:272.
Southern, E.M. (1975). Detection of specific sequences among DNA fragments separated by gel electrophoresis. J. Mol. Biol., 98,503-17
Thiede HA, Creasman WT, Metcalfe S. (1966) Antenatal analysis of the human chromosomes. Am J Obstet Gynecol 1966;94:589.
Valenti, C. (1972) Endoamnioscopy and fetal biopsy: a new technique. American Journal of Obstetrics and Gynecology, 114,561
Valenti, C. (1973) Antenatal detection of hemoglobinopathies. American Journal of Obstetrics and Gynecology, 115,851
Ward RHT, Model B, Petrou M, et al (1983) Method of sampling chorionic villi in first trimester of pregnancy under guidance of real time ultrasound. Br Med J 286:1542
Westin, B. (1954). Hysteroscopy in early pregnancy. Lancet, 11,872
Back to History of Ultrasound in Obstetrics and Gynecology.
The first use of amniotic fluid examination in the diagnosis of genetic disease was reported by Fuchs and Riis in 1956 in their seminal article in "Nature". They determined fetal sex from cells found in amniotic fluid, basing on the presence or absence of the Barr body. John Edward in England, also discussed for the first time in 1956 the possibility of the "antenatal detection of hereditary disorders". The determination of fetal sex led to the prenatal management of patients with Haemophilia A in 1960, and Duchenne muscular dystrophy in 1964.

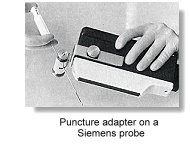
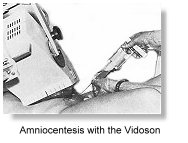 As early as 1967, and basing on the Vidoson, Hofmann and Hollander in Germany had discussed the importance of placental localization using ultrasound before amniocentesis. Jens Bang and Allen Northeved in Copenhagen described ultrasound-guided amniocentesis in 1972. In the mid 1970s to early 80s, genetic amniocentesis was largely performed under static B-scan ultrasound guidance. An ultrasound scan was performed to locate a feasible pocket of amniotic fluid before a tap, which was done basically without actually seeing the needle tip going into the fluid pocket. With the advent of real-time scanners, a small number of centers had in the late 1970s started to perform amniocentesis by simultaneously visualizing the puncture needle tip on the scanner monitor. One such pioneer was the Birnholz group at Harvard who used an early phased array for the purpose.
As early as 1967, and basing on the Vidoson, Hofmann and Hollander in Germany had discussed the importance of placental localization using ultrasound before amniocentesis. Jens Bang and Allen Northeved in Copenhagen described ultrasound-guided amniocentesis in 1972. In the mid 1970s to early 80s, genetic amniocentesis was largely performed under static B-scan ultrasound guidance. An ultrasound scan was performed to locate a feasible pocket of amniotic fluid before a tap, which was done basically without actually seeing the needle tip going into the fluid pocket. With the advent of real-time scanners, a small number of centers had in the late 1970s started to perform amniocentesis by simultaneously visualizing the puncture needle tip on the scanner monitor. One such pioneer was the Birnholz group at Harvard who used an early phased array for the purpose. 

 Valenti in 1973 used the 'endoamnioscope' and reported the first aspiration of fetal blood and the diagnosis of haemoglobinopathy. The newer Dyonics® Needlescope became available in the following year, which was 1.7mm in diameter with a 2mm cannula. General anaesthetics was not required for its use.
Valenti in 1973 used the 'endoamnioscope' and reported the first aspiration of fetal blood and the diagnosis of haemoglobinopathy. The newer Dyonics® Needlescope became available in the following year, which was 1.7mm in diameter with a 2mm cannula. General anaesthetics was not required for its use. 
 In 1977, Hobbins and Mahoney reported successful exclusion of beta-thalassemia and diagnosis of sickle cell disease without aparent risk to the mother and fetus. Other important workers included Alter and Nathan, and Fairweather in London. Rodeck and Campbell reported the diagnosis of spina bifida using this method. In 1979 the group reported a success rate of obtaining pure blood samples of 94% in 51 attempts. They introduced the method of aspirating from one of the larger vessels at the base of the cord. Most investigators started with the diagnosis of haemoglobinopahies, in which maternal cell contamination did not affect the accuracy of the results
In 1977, Hobbins and Mahoney reported successful exclusion of beta-thalassemia and diagnosis of sickle cell disease without aparent risk to the mother and fetus. Other important workers included Alter and Nathan, and Fairweather in London. Rodeck and Campbell reported the diagnosis of spina bifida using this method. In 1979 the group reported a success rate of obtaining pure blood samples of 94% in 51 attempts. They introduced the method of aspirating from one of the larger vessels at the base of the cord. Most investigators started with the diagnosis of haemoglobinopahies, in which maternal cell contamination did not affect the accuracy of the results Other reported diseases diagnosed via fetoscopy included haemophilia (1979, Firsheim), chronic granulomatous disease (1979, Newburger), galactosaemia (1979, Fensom), and Tay-Sachs disease (1979, Perry). Fetal skin biopsy successfully diagnosed congenital bullous ichthyosiform erythroderma ichthyosis by the
Other reported diseases diagnosed via fetoscopy included haemophilia (1979, Firsheim), chronic granulomatous disease (1979, Newburger), galactosaemia (1979, Fensom), and Tay-Sachs disease (1979, Perry). Fetal skin biopsy successfully diagnosed congenital bullous ichthyosiform erythroderma ichthyosis by the  Fetoscopic guided Laser occlusion of chorioangiopagous vessels (FLOC) was first pioneered by De Lia in 1988 at the University of Utah for the treatment of the Twin-to-Twin-Transfusion Syndrome (TTTS) .
Fetoscopic guided Laser occlusion of chorioangiopagous vessels (FLOC) was first pioneered by De Lia in 1988 at the University of Utah for the treatment of the Twin-to-Twin-Transfusion Syndrome (TTTS) . 
 In 1968 Mohr in Scandinavia introduced the concept of antenatal genetic diagnosis using sampled chorionic villi. He performed transcervical biopsy of the chorion under direct endoscopic vision, using a straight 5mm endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding, infection and failed culture. The approach was slowly abandoned in the midst of increasing safety from mid-trimester amniocentesis. Kullander and Sandahl in 1973 and Hahnemann in 1974 reported fetal chromosome analysis from transcervical placental biopsy prior to termination in early pregnancies. The first successful prenatal diagnostic use of chorionic villi biopsy was apparently reported in 1975 from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China, where fetal sex was diagnosed for the purpose of sex pre-selection. This was reported in the first issue of the (new) Chinese Medical Journal. They performed blind aspirations using a 3mm metal cannula on a group of 100 patients. When a soft resistence was met, a smaller internal tube was advanced further and placental material obtained by syringe suction. They claimed to have 6 wrong diagnosis out of 99 successful attempts and only 4 prenatal losses. Investigators in the United States were, however unable to duplicate the results and the idea of first trimester antenatal diagnosis was again shelfed for some time.
In 1968 Mohr in Scandinavia introduced the concept of antenatal genetic diagnosis using sampled chorionic villi. He performed transcervical biopsy of the chorion under direct endoscopic vision, using a straight 5mm endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding, infection and failed culture. The approach was slowly abandoned in the midst of increasing safety from mid-trimester amniocentesis. Kullander and Sandahl in 1973 and Hahnemann in 1974 reported fetal chromosome analysis from transcervical placental biopsy prior to termination in early pregnancies. The first successful prenatal diagnostic use of chorionic villi biopsy was apparently reported in 1975 from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China, where fetal sex was diagnosed for the purpose of sex pre-selection. This was reported in the first issue of the (new) Chinese Medical Journal. They performed blind aspirations using a 3mm metal cannula on a group of 100 patients. When a soft resistence was met, a smaller internal tube was advanced further and placental material obtained by syringe suction. They claimed to have 6 wrong diagnosis out of 99 successful attempts and only 4 prenatal losses. Investigators in the United States were, however unable to duplicate the results and the idea of first trimester antenatal diagnosis was again shelfed for some time.
 In 1983, Ward in London performed transcervical chorionic sampling under ultrasonic guidence using a 1.5 mm malleable polyethylene catheter and syringe suction. His group reported 67% sampling success rate, including 7 patients for the diagnosis of haemoglobinopathies. The Brambati group in Milan demonstrated in 1983 that with ultrasonic guidance, success rate of obtaining chorionic material rose from 75% to 96%. Brambati used a 1.5mm polyethylene tube with a soft stainless steel malleable obturator inserted into the 1 mm internal barrel. This design has been the most common design in use today. Other workers like Dumez in Paris used a simple 2 mm biopsy forceps. The Simoni and Brambati group in Milan described in 1983 a technique for direct chromosome and biochemical analysis on first trimester chorionic villi (direct prep), without preliminary culture. Chorionic villi were obtained by aspiration or direct biopsy from the chorion frondosum, at the edge of the placental disc. The inner cytotrophoblastic layer beneath the outer syncytiotrophoblast layer contains actively mitotic cells in freshly sampled villus which could be recovered with their technique. Virtually all analyses could be performed with these fresh whole villus.
In 1983, Ward in London performed transcervical chorionic sampling under ultrasonic guidence using a 1.5 mm malleable polyethylene catheter and syringe suction. His group reported 67% sampling success rate, including 7 patients for the diagnosis of haemoglobinopathies. The Brambati group in Milan demonstrated in 1983 that with ultrasonic guidance, success rate of obtaining chorionic material rose from 75% to 96%. Brambati used a 1.5mm polyethylene tube with a soft stainless steel malleable obturator inserted into the 1 mm internal barrel. This design has been the most common design in use today. Other workers like Dumez in Paris used a simple 2 mm biopsy forceps. The Simoni and Brambati group in Milan described in 1983 a technique for direct chromosome and biochemical analysis on first trimester chorionic villi (direct prep), without preliminary culture. Chorionic villi were obtained by aspiration or direct biopsy from the chorion frondosum, at the edge of the placental disc. The inner cytotrophoblastic layer beneath the outer syncytiotrophoblast layer contains actively mitotic cells in freshly sampled villus which could be recovered with their technique. Virtually all analyses could be performed with these fresh whole villus.